+44 (0)1983 534373 [email protected]
History
 Interest in chest disease and allergy is not new to the Isle of Wight. In the nineteenth century, Hill Hassall founded the Hospital for Disease on the Lungs, subsequently the Royal National Hospital for Disease of the Chest, in Ventnor.
Interest in chest disease and allergy is not new to the Isle of Wight. In the nineteenth century, Hill Hassall founded the Hospital for Disease on the Lungs, subsequently the Royal National Hospital for Disease of the Chest, in Ventnor.
Professor Carl Prausnitz in 1921 had made the crucial observation that the blood of an allergic individual contained a transferable factor, subsequently shown to be an antibody. Prausnitz moved from the University of Breslau in 1933 and two years later became a general practitioner on the Isle of Wight in his mother’s home village of Bonchurch, where he practiced as Dr. Carl Prausnitz Giles until his death in 1963. Thus the Island has a strong link with a father figure of allergy and immunology.
The Isle of Wight District Health Authority approved the establishment of a clinical allergy service at St Mary’s Hospital in 1979. At this time the prevalence of allergic conditions in all children born on the Isle of Wight in 1977 was being recorded.
An increasing research commitment was recognised in 1988 when accommodation was made available at Frank James Hospital, East Cowes, for a small Clinical Allergy Research Unit which was opened by Professor Stephen Holgate. A full-time fellow in clinical allergy, Dr Hasan Arshad, was appointed and the research output increased significantly. Dr Arshad gained an MD for his research with the Isle of Wight birth cohort and the 1990 Allergy Prevention Study.
In 1991 the Unit moved to temporary accommodation at St. Mary’s Hospital in Newport. Dr David Hide’s retirement from his position as paediatrician and appointment as part-time consultant in clinical allergy, helped the development of allergy and enabled the staff of the Unit to begin planning a purpose-built asthma and allergy research centre. It was realised that the National Health Service was unlikely to cover the capital costs of such an unusual venture so members of the Unit commenced fund raising. In 1994 the building of the Centre became a reality and staff moved into their new Research Centre in September 1995. Unfortunately, Dr David Hide died in March 1996 before the official opening of the Centre by HRH Duchess of Gloucester in July 1996.
In April 1997 Dr Hasan Arshad was appointed Director of The David Hide Asthma and Allergy Research Centre by the Board of Trustees.
In 2004 Dr Graham Roberts joined the research team, working alongside Dr Arshad as Co-Director.
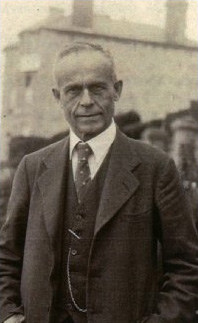
 Dr David Wallace Hide
Dr David Wallace Hide
by Eric Trimmer, British Journal of Clinical Practice,
June 1996
David Hide was the sort of person that the late Sir Clement Price-Thomas used to describe as a ‘proper doctor’. Although eminent in his field of practice, David never retreated into the ivory tower of ultraspecialisation and remained, at heart and in practice, a kindly and approachable physician. Children – those most perceptive of patients – seemed to realise that, even in the worrying situations they had to face in hospital, they had a trusted friend and kindly ally in their doctor David.
David Hide was very much a ‘homegrown’ product. Born in Portsmouth, he was educated at Portsmouth Grammar School, near the Cathedral, in the old town. He enjoyed his medical education as an undergraduate at Bristol University, and qualified in 1961. His early choice of postgraduate experience in Bristol, Oxford and Swindon was directed towards a career in paediatrics, an ambition that bore fruit when he was appointed consultant paediatrician to the (old) Royal Isle of Wight Hospital. There, in Ryde – just over the Solent from his ‘Pompey’ birthplace – he set to work putting the specialty of paediatrics and neonatal medicine on a sound and progressive basis for the Island. When the Royal Isle of Wight Hospital made way for the new St Mary’s Hospital at Newport, David Hide became its first paediatric physician.
In 1992 David Hide was appointed by the Wessex Regional Health Authority as a non-executive director of the newly established St Mary’s Hospital NHS Trust. This was something of a watershed since it marked the end of his career as a clinical paediatrician, but he did maintain a strong link with the world of paediatrics through his appointment to Senior Lecturer in Child Health at the University of Southampton. Election to the Fellowship of the Royal College of Physicians followed his appointment to Director of Clinical Allergy at St Mary’s, by which time he was a world figure in the field of clinical allergy.
David Hide was a man of sound clinical insight and considerable perspicacity. He had the courage to express his conviction that there was such a condition as ‘good allergy’ at a time when most physicians were convinced that such a diagnosis was more than suspect. His research in the field of clinical allergy, begun in the 1970s was at last becoming widely noticed and appreciated – he achieved a National Distinction Award. Always very much a research oriented physician, he was largely instrumental in furthering the concept of a research and development unit at St Mary’s with the prime aim of providing help and support for staff at the hospital whose ambitions included clinical research projects.
But the main memorial to David Hide must be The Asthma and Allergy Research Centre at St Mary’s. This is already operational, but due to be opened formally by the Duchess of Gloucester this July. Sadly, David will not be present. He never spared himself, despite a warning that his cardiovascular pathology was already making itself felt. He remained a dedicated publicist of the contribution to ill health that atopy makes to many young and not so young lives. Within hours of his premature death at the age of 58, he had been speaking on the adverse reactions of peanuts on youngsters in Britain today. Only a few days before that he had once again been supporting the National Asthma Campaign’s annual conference at Leicester.
David Hide’s much loved research had, for the past eight years, been focused on antigen avoidance as a modus operandi in the management of atopic disease – a therapeutic intervention of considerable moment. His careful research had shown that antigen avoidance could bring about substantial reduction in the atopic response. Of more recent interest, perhaps, his research also involved assessment of the use of commercial air-filtration techniques in the management of both asthma and allergic rhinitis.
Enthusiasm, integrity and friendliness are the words that spring to mind when we try to describe David Hide, and I consider myself lucky to have experienced these aspects of his personality personally when I asked him to join the Editorial Board of the British Journal of Clinical Practice.
One of the legacies of this man that we must not forget is the personal demonstration he gave to young men and women starting off in medicine that it is neither necessary to go to a fashionable public school nor qualify at Oxbridge, London or Edinburgh to go on to a life of professional excellence and become an acknowledged expert, both locally and internationally, in your chosen field. David Hide also demonstrated personally that a mid-career break in medical practice can bring great rewards to both medicine and patients.
David Wallace Hide probably did not take enough time off to enjoy his activities at the Isle of Wight Health Associates Cricket Club or his golf at Freshwater Bay. He will be greatly missed at St Mary’s and by his wife, three children and brother.”
An excerpt from an article in the Isle of Wight Public Health Report written by David Hide shortly before his death.
“The staff of The David Hide Asthma and Allergy Research Centre are very keen to secure the future of the Centre. First and foremost they wish to provide a high quality clinical allergy referral service for the Isle of Wight and for mainland medical practitioners and patients who wish to use it. They also believe that some of the research that is already in progress, and other projects for which funding is being sought, are of cardinal importance to the many who suffer allergic disease and may play a significant role in reducing the enormous cost to the health services of this and other countries, of conditions such as asthma.
The Isle of Wight does not have to have an Asthma and Allergy Centre. However it has been proved over the last 20 years that medical advances are not the exclusive province of universities and medical schools. Substantial contributions to knowledge can be made by a closely integrated population where health professionals and lay community understand their mutual objective.
The Centre is now a fact of medical life on the Isle of Wight. If it can continue to provide an effective clinical service and maintain an output of high quality research it will hope to continue to receive the support of the public, purchasers and those who allocate research funding”
